November 26, 2021 The ABCs of Varicose Veins

Varicose veins are a common health condition. According to the Canadian Society for Vascular Surgery, varicose veins affect up to 20% of the adult population. Women tend to be more prone to varicose veins than men. But other risk factors may also contribute to developing varicose veins. These include obesity, older age, pregnancy, a family history of varicose veins, and others. For the most part, varicose veins are not considered a serious medical condition but they can cause pain and discomfort. And in some instances, they may lead to more serious problems. Read on to discover everything you should know about varicose veins: the causes, symptoms, diagnosis, treatments, and how to prevent them.
What are varicose veins?
Varicose veins, also known as varicosities, are enlarged and twisted veins. They occur when veins become dilated and overfill with blood. They most often appear in the legs, typically in the thighs, ankles, and feet. Varicose veins are usually blue or purple in colour and will appear swollen and raised.
What about spider veins?
Spider veins are a form of varicose veins that look like a sunburst or spider’s web. They are smaller than varicose veins and often appear on the face and legs, just under the skin. Spider veins are also blue or purplish in colour but do not protrude or bulge like varicose veins.
What causes varicose veins?
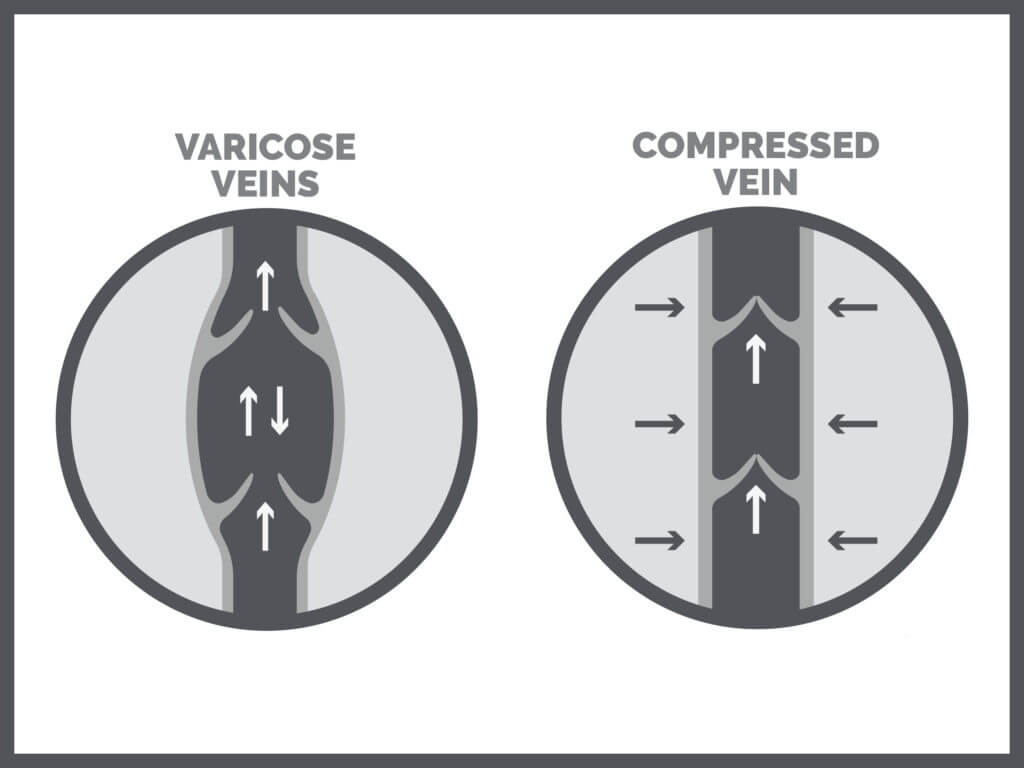
Varicose veins occur because veins are not functioning properly. To ensure blood flows back to your heart, veins have one-way valves to prevent the blood from flowing backwards. If these valves are damaged or weakened, blood can leak back into the lower part of the vein. This then causes the vein to swell, as over time blood will get stuck there. Sitting or standing for long periods can cause blood to pool in the legs and put extra pressure on the veins. This heightened pressure may then cause the vein to stretch and weaken its walls and valves.
Risk factors for varicose veins
While varicose veins are sometimes hereditary and more common in some families, other risk factors come into play. These include:
- Age (varicose veins are most common in women over 50)
- Being overweight or obese
- Leading an inactive lifestyle
- Standing or sitting for long periods
- Being female
- Pregnancy
- Smoking
- Leg injury
- Taking oral contraceptive pills or hormone replacements
- Frequent air travel (airline crews)
What are the symptoms of varicose veins?
Typically, varicose veins will manifest as very visible, misshapen veins on the legs that are blue or purple in colour. You may also experience pain, swelling, achiness, a burning sensation, or a feeling of heaviness. Other common symptoms include: colour changes in the skin, rash, and sores on the legs. Severe varicose veins can lead to more serious skin conditions such as ulcers or non-healing sores. However, everyone experiences symptoms differently so it is always important to speak with your doctor for proper diagnoses.
How to diagnose varicose veins?
If you have any of the symptoms above or suspect you have varicose veins, it is important to speak with your doctor. Normally, your doctor will take a full medical history, ask about pain and other symptoms, and examine your legs and veins. Usually, an ultrasound will be used to check blood flow in your legs. This is a non-invasive and painless test. In some cases, depending on where the varicose veins are located, your doctor may also do a venogram. Here, a special dye is injected into your veins and X-rays of the area are taken. The dye allows your doctor to see how blood is flowing.
Both the ultrasound and venogram are used to rule out blood clots, blockages, or other disorders that may be causing the swelling or pain.

Are varicose veins dangerous?
For the most part, varicose veins are not considered a serious medical condition. While they may cause pain, swelling, and discomfort, doctors are usually conservative in their treatment. However, as mentioned above, severe varicose veins can lead to skin condition such as ulcers and non-healing sores. In rarer cases, there is a small chance of developing a blood clot in the deep vein. Blood clots need immediate medical care. The danger with blood clots is that a piece of the clot can break off and travel through your veins to the lungs. This is known as a pulmonary embolism and is very serious. But note, deep vein thrombosis does not usually happen with varicose veins.
What are the treatments for varicose veins?
How varicose veins are treated will be determined by your healthcare provider. It will also depend on your age, medical history, lifestyle, overall health, severity, signs and symptoms, among others. However, common treatments include:
- Elevating the legs above the heart three to four times a day for 15 minutes. This can help relieve symptoms and reduce swelling.
- Lifestyle changes such as losing weight, exercising more, avoiding standing or sitting for long periods, and so on.
- Compression stockings are used to squeeze the veins and prevent blood from pooling in the legs. This can be quite effective if worn daily. This is a non-invasive treatment and easily adopted into your lifestyle since you can replace your existing socks for compression socks.
- Sclerotherapy: a saline solution is injected into the veins, which means they no longer carry blood and other veins take over.
- Thermal ablation: a laser or radio frequency energy is used to destroy the vein wall.
- Vein stripping: this is a surgery to remove the vein.
- Microphlebectomy: small incisions are made to remove the varicose veins.
Compressing stockings to prevent and treat varicose veins
If you have varicose veins or spider veins, wearing compression socks can help reduce the appearance and prevent new ones from appearing. It takes only five days of consistent wear for visible results! Basically, by applying gentle pressure to the legs, compression socks or stockings improve the work of veins and help blood flow back to the heart. As such, they help blood vessels work better, prevent swelling, and reduce pain. This in turn promotes better blood circulation: blood flows more freely and the arteries, which carry oxygen-rich blood to the muscles, can relax. And this helps prevent blood from refluxing down toward the feet or clotting.
Compression socks are commonly prescribed for varicose veins. These socks or stockings come in different compression levels, measured in millimetres of mercury (mmHG). For varicose veins, doctors will typically recommend compression between 20–30 mmHG and 30–40 mmHG. Always consult your doctor to know which compression level is best for you.
Other things you can do to prevent varicose veins
In addition to wearing compression socks or stockings, you can take certain steps to help prevent varicose veins. These include:
- Maintaining a healthy weight
- Exercising regularly
- Avoiding crossing your legs when sitting
- Not wearing tight clothing
- Not sitting or standing for long periods
- Putting your feet up while sitting
- When flying, stay hydrated and make sure to stand and stretch frequently
Varicose veins are a common health condition that affects up to 20% of the adult population in Canada. While they are not considered a serious medical condition, you should still consult with your doctor if you have symptoms of varicose veins. To help treat and improve their appearance, wearing compression socks is recommended. You will see visible results in just five days of consecutive wear. Always check with your doctor or healthcare provider to know which compression level is best for you. Shop Supporo’s wide range of comfortable, high-quality compression socks today.